What is chromosome?
What is chromosome?
- TOP
- Fetal Medicine
- What is chromosome?
What is a chromosome?
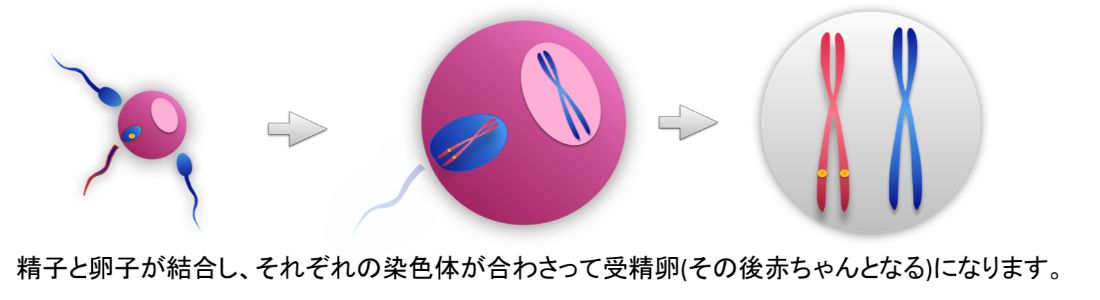
The sperm and the egg combine, and the chromosomes of each combine to form a fertilized egg (and subsequently a baby).
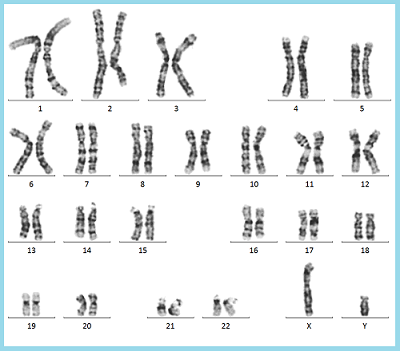
Chromosomes are like a ship with genetic information inherited from our parents. A person has 46 chromosomes (23 pairs), which are divided into 44 (22 pairs) autosomes and 2 (1 pair) sex chromosomes.
Chromosomes cannot be acquired, so even if an abnormality is found, for example, a high or low number of chromosomes, it cannot be treated.
Trisomy 21 (Down Syndrome)
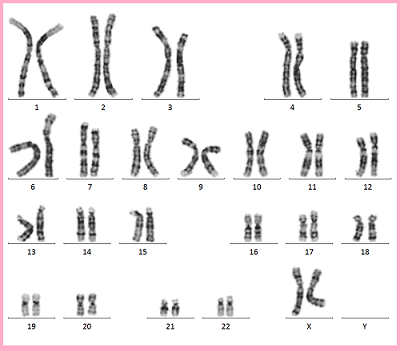
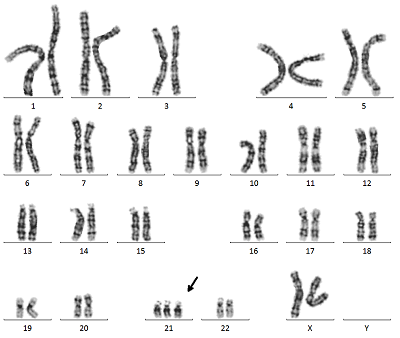
Trisomy 21 is a congenital disorder in which the 21st chromosome is one chromosome too many. It is a commonly known chromosomal abnormality and is also called “Down Syndrome”. In most cases, Down syndrome is not inherited from a particular mom and dad, and any mom and dad can have a child with Down syndrome.
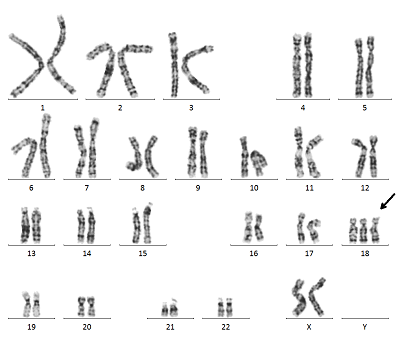
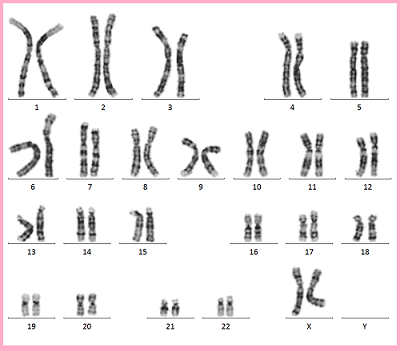
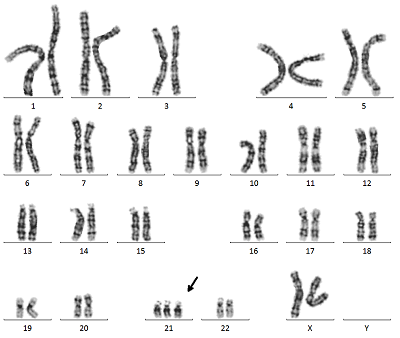
Chromosomes 1 through 22 are paired with two chromosomes, one inherited from mom and one from dad, but chromosome 21 has three chromosomes, one more than the other, which is characteristic of Down syndrome chromosomes (Figure 1).
※click
Translocation type Down syndrome is born when the mother or father has a special chromosome structure called Robertson translocation. In this case, the chances of being born with Down syndrome are higher.
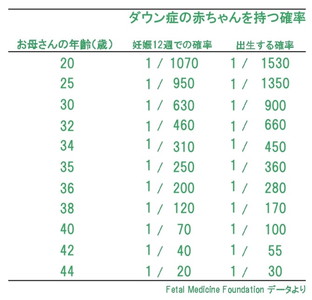
However, the age of the mother is said to have an effect on the incidence of Down syndrome. It is said that the older the mother, the higher the incidence of Down syndrome (Figure 2). In Korea and other countries, many facilities recommend CVS and Amniocentesis for all women who deliver at the age of 35 or older.
In Japan, many women with older pregnancies are concerned, but only a small percentage of them undergo testing.
※click
18 Trisomy (Edwards syndrome)
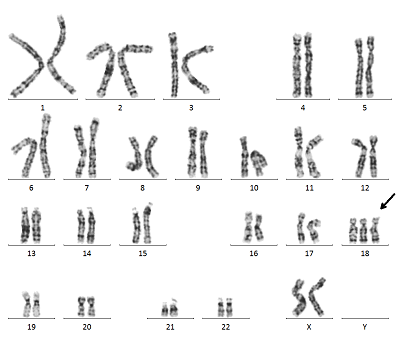
Trisomy 18 is a congenital chromosomal abnormality in which there is one more chromosome than normal in the 18th chromosome, also known as Edwards syndrome.
Trisomy 18 is more likely to occur in girls, who are about three times more likely to have it than boys. The overall chance of occurrence for girls and boys combined is about 1 in 3,500 to 8,500. More than 90% of babies with 18-trisomy have miscarriages or die within the first year of life due to congenital diseases occurring during pregnancy. However, there are some people with 18 trisomy who live a healthy life (many are mosaic), so it is impossible to say how long they will live.
Babies with trisomy 18 show physical characteristics such as “stunted growth, small jaw, low ears, overlapping fingers, and contractures of the limbs” from the beginning of pregnancy, and the possibility of cardiac malformations is also quite high, and the brain maldevelopment are often seen. These features are observed as very characteristic findings in the early fetal diagnosis.
Trisomy 13 (Patou syndrome)
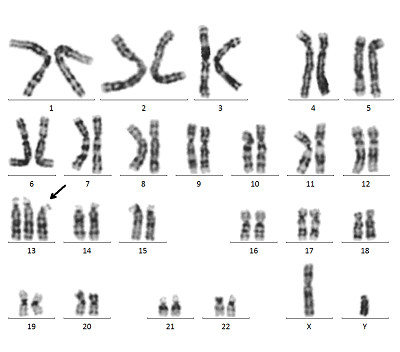
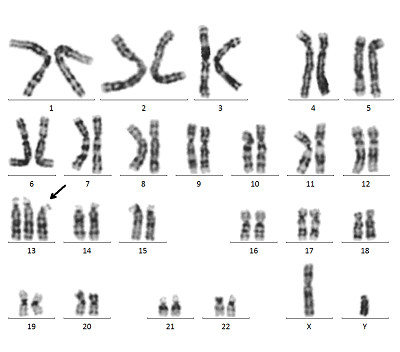
Trisomy 13 is a congenital chromosomal abnormality in which the 13th chromosome is one chromosome too many, also known as “Patou syndrome”.
Trisomy 13 occurs in approximately one in 5,000 to 12,000 children. This chromosomal abnormality is characterized by symptoms that tend to appear in the head, such as microcephaly, holoprosencephaly, microphthalmia, nose abnormalities, cleft lip and palate, cardiac malformations, kidney abnormalities, and polydactyly or polydactyly on the little finger side.
Tachycardia is also a common feature in early pregnancy. Many Trisomy 13 babies die in the mother’s womb during early pregnancy. Other symptoms such as small polydactyly, inguinal hernia, single palmar line, and severe mental retardation may also occur. Early fetal diagnosis is often easier to detect because babies with Trisomy 13 have many characteristic findings.
Turner Syndrome (45,X)
Turner syndrome is a chromosomal abnormality in girls caused by a partial or total deletion of one of the two X chromosomes.
Turner syndrome occurs in about one case per 1,000 to 2,000 children. Physical characteristics include short stature, sagging of the skin on the back of the neck, and often no secondary sexual characteristics are seen even at the age of puberty.
In addition, the symptoms of Turner syndrome can vary from mild to severe. Many babies who are born at 10 months are unaware that they have Turner syndrome. In most cases, the symptoms are only mild in the neonatal stage.
However, in childhood, symptoms such as short stature and, in adolescence, “failure to develop breasts and uterus” appear.
In many cases, treatment such as the administration of growth hormones or female hormones is necessary. However, many people with Klinefelter’s syndrome have good intellectual development, and some of them go on to become doctors, nurses, or other intellectual professionals.
Klinefelter’s syndrome (47,XXY)
Klinefelter’s syndrome is an abnormality in the number of chromosomes in boys caused by hyperplasia of the sex chromosomes. In a normal boy, the only sex chromosome responsible for determining gender is XY, but in Klinefelter’s syndrome, excessive X chromosomes such as XXY and XXXY are formed.
Klinefelter’s syndrome is known to occur at a high frequency among chromosomal abnormalities, with a rate of about one case per 500 boys.
This chromosomal abnormality rarely causes any apparent symptoms, such as tall, long arms and legs or poor muscle tone. However, in some cases, symptoms such as gynecomastia, beard and pubic hair loss may occur due to decreased production of the male hormone testosterone. In fact, it is said that many people spend their entire lives unaware that they have Klinefelter’s syndrome, even in adulthood.
In most cases, there is no problem with intellectual development, and it is often discovered only after the couple gets married and undergoes a chromosome test at a fertility treatment facility to investigate the cause of infertility.
Microchromosome abnormalities (microdeletions and microduplications) can occur in all chromosomes
Microchromosome abnormalities (microdeletions and microduplications) can occur anywhere on all chromosomes.
A microchromosome deletion or duplication can occur when one of the parents has a deletion or duplication in the same region, in which case it is “benign” and there are no pathological symptoms.
Depending on the location of the microchromosome abnormality, the gene carrying the abnormality may be different, so whether or not the abnormality will actually cause pathological symptoms cannot be determined until a detailed examination is done.
In some cases, the microchromosome abnormality occurs only in the placenta and the baby has no problem at all, so a SNPmicroarray test using an Amniocentesis is necessary to confirm this.
Some facilities offer NIPT to check for microchromosomes, but it can also indicate microdeletions or duplications in the mother. Please note that the degree of resolution of microchromosome tests varies.
How are fetal chromosomes examined?
There are two types of fetal chromosome tests: the CVS and the Amniocentesis, both of which can eventually test all the chromosomes.
When checking chromosomes that are prone to abnormalities, the QF-PCR method can determine the number of chromosomes with 21 trisomy, 18 trisomy, and 13 trisomy in a day. However, CRIFM will be using the D-karyo (digital chromosome) test starting in 2020 to detect microchromosomal abnormalities that are missed by the conventional CVS and Amniocentesis. The D-karyo (digital chromosome test) will be available from 2020.
In addition, SNPmicroarray can reveal more detailed microchromosomal abnormalities and abnormalities such as uniparental disomy. In addition, genetic testing (targeted exome sequencing and Sanger testing) can reveal congenital abnormalities caused by genetic mutations.
QF-PCR, G-band, and D-karyo are included in the standard CVS and Amniocentesis, so that all patients can be checked for microchromosomal abnormalities in all chromosomes. As an option, SNPmicroarray test is available.
The SNP microarray test is useful for patients who have undergone pre-implantation genetic tests (PGT, chromosome testing of eggs prior to implantation into the uterus through IVF). Genetic testing is also available for those who are suspected of having genetic mutations on ultrasound.
In any case, a detailed explanation and consent is required at a genetic counseling session, and the test is not available to everyone.
For more information on the CVS and Amniocentesis, click here.
QF-PCR method
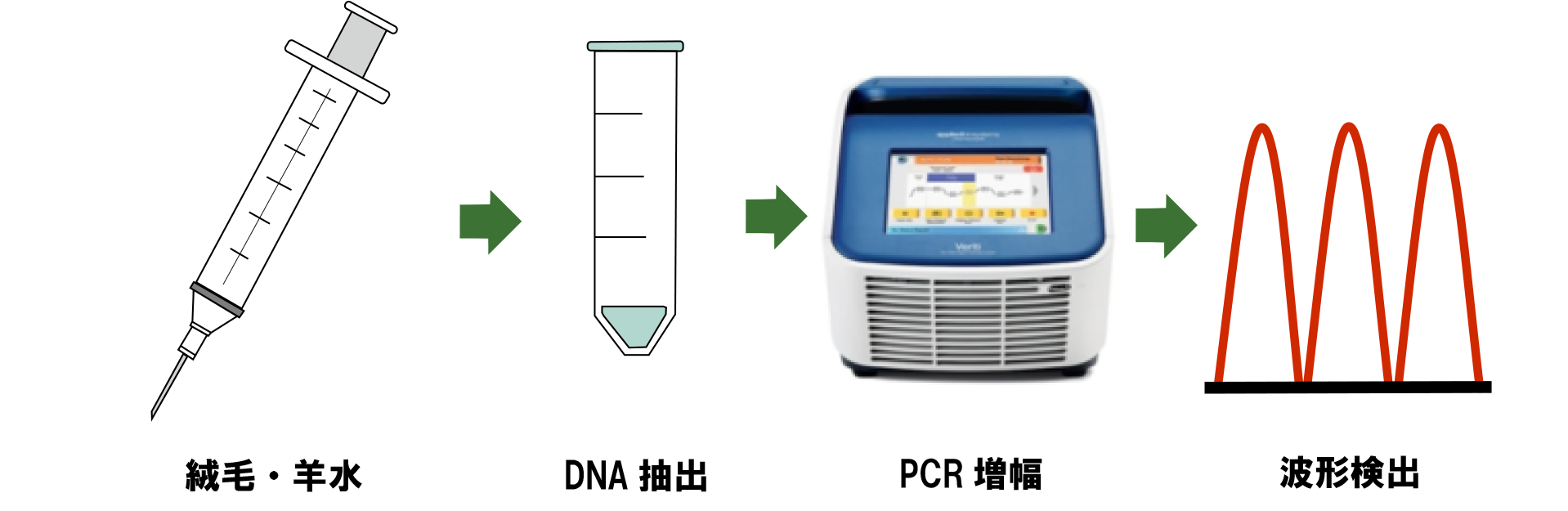
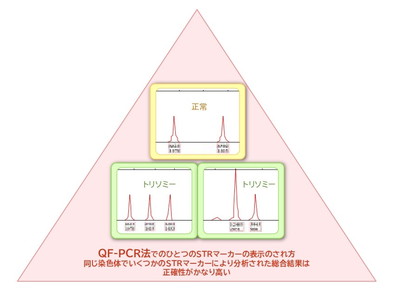
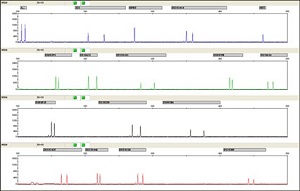
This test extracts DNA from chorionic villi and amniotic fluid to detect 21-trisomy, 18-trisomy, 13-trisomy, X and Y abnormalities, which are prone to chromosomal abnormalities. Several unique and specific STR markers present in chromosomes are simultaneously amplified and analyzed to quantitatively indicate whether the chromosome is a trisomy or not (Figure 3).
※click
In Japan, the FISH method has been used for rapid testing for a long time, but the QF-PCR method uses several STR markers on a single chromosome to make a comprehensive judgment (Figure 4), which is not only more accurate, but also shortens the testing time and enables simultaneous testing of multiple samples. The QF-PCR method is the first choice in Europe, Canada, and many Asian countries, and CRIFM has also adopted the rapid and accurate QF-PCR test method since 2009.
※click
G-band chromosome test (traditional analog chromosome analysis)
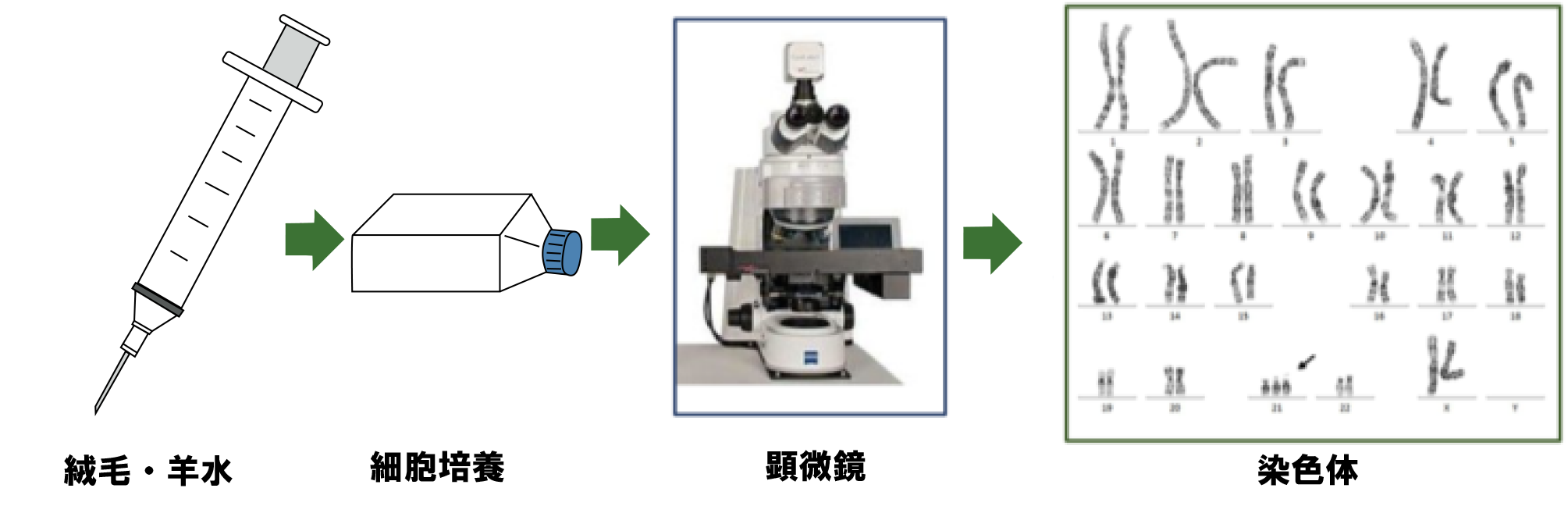
This test is performed by culturing fetal cells from chorionic villi or amniotic fluid to examine the shape and number of all chromosomes. The test can detect most of the changes in chromosomes, but cannot detect minute changes or changes at the genetic level.
The test results are returned in the form of chromosomes arranged in number order. The test results are returned with chromosomes arranged in number order.
Even if the CVS or Amniocentesis shows a normal G-band, microchromosomal abnormalities may be detected after birth because of the limitations of prenatal G-band. In CRIFM, D-karyo (described below) is performed at the same time to compensate for the weakness of the G-band.
D-karyo (the latest digital chromosome) test
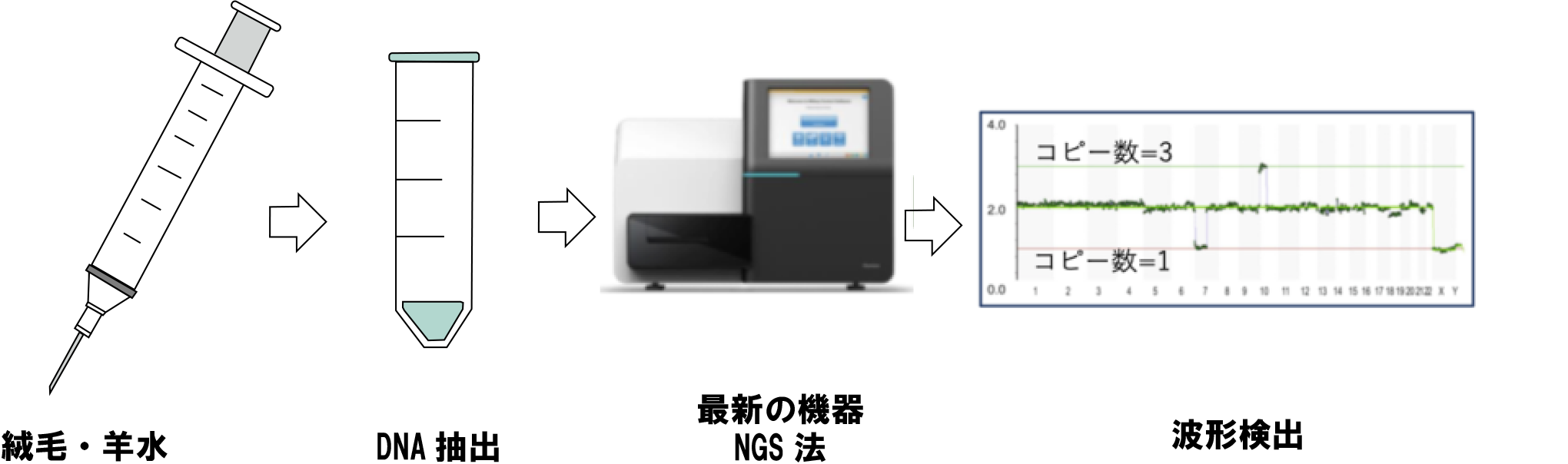
D-karyo analysis is the latest chromosome analysis method using the next-generation sequencing method developed in 2020 (*), and as of April 2021, only CRIFM is offering this excellent method in Japan.
D-karyo is an abbreviation for digital chromosome analysis, and is an analysis method that can reveal minute changes in chromosomes that cannot be observed with a microscope by detecting the increase or decrease in the amount of DNA contained in the chromosomes.
In this method, DNA is extracted from the collected villi and amniotic fluid, converted into digital data using a device called a next-generation sequencer (NGS), and microchromosomal abnormalities and partial mosaics are detected by using several special software programs.
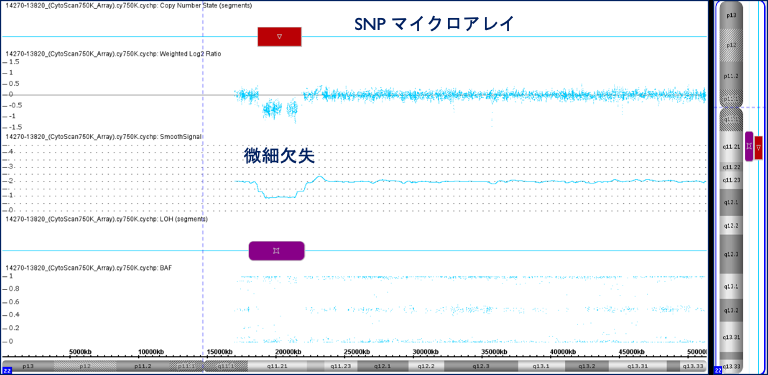
However, since D-karyo analysis is a screening analysis, if a positive result is obtained by D-karyo, SNP microarray analysis including that of both parents will be required to determine the exact location and the impact of the change on the fetus.
※Shimokawa, Pooh, et al. D-karyo—A New Prenatal Rapid Screening Test Detecting Submicroscopic CNVs and Mosaicism. Diagnostics. 2021; 11(2):337. https://doi.org/10.3390/diagnostics11020337
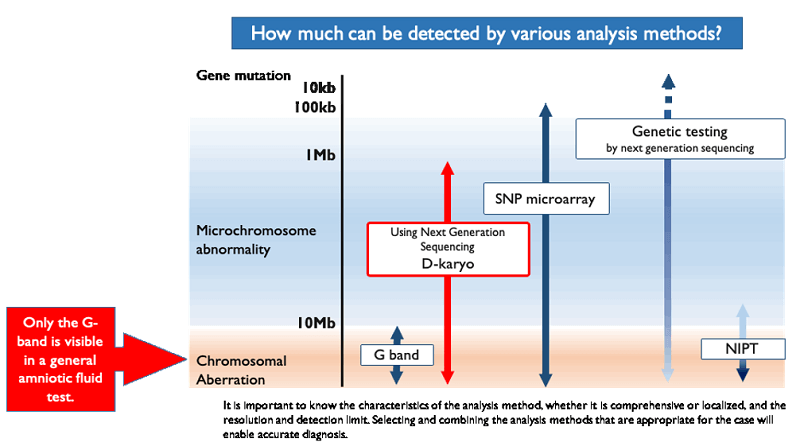
SNPmicroarray test
Unlike conventional chromosome tests, SNP microarray is an analysis method that can reveal small changes in chromosomes that cannot be observed under a microscope by detecting whether the amount of DNA contained in the chromosome is increasing or decreasing.
SNP microarray analysis can detect an increase or decrease in the amount of DNA, which means that it can detect the absence of very small data on a chromosome or a slight increase in data. In other words, SNP microarray analysis can detect even the most minute of microchromosomal abnormalities.
It is also possible to detect cases in which a part of a chromosome is derived from only one parent (uniparental dichotomy), whereas normally a pair of chromosomes is inherited from both father and mother.
To detect the possibility of a congenital disease even if the chromosomes are normal
Even if your chromosomes are normal, it is possible that you have a congenital disease of the heart or other organs. If anything, the probability may be higher.
For this reason, the CRIFM Prenatal Medical Clinic performs a full body organ check on the baby by about 20 weeks of pregnancy. We check the baby’s entire body for 30 items, from the detailed structure of important organs such as the brain and heart to the bones of the fingers, nose, and lips, so that the mother can have a safe pregnancy.
Recently, some of the abnormalities in brain development can be detected as early as 20 weeks of pregnancy, and CRIFM has a fetal brain center, and our strength is that we perform a fetal brain dock for all pregnant women in mid-term fetal diagnosis.
If an abnormality is found in the fetal diagnosis, we will provide the mother and father with an explanation based on the latest medical information, such as what kind of disease it is, how serious the condition is, whether there are any treatment options, and how to proceed with the treatment.
For more details, please see the “fetal diagnosis” page.
