What is NIPT?
What is NIPT?
- TOP
- Fetal Medicine
- What is NIPT?
NIPT is a genetic test that aims to measure fetal DNA in maternal plasma. However, NIPT does not detect all abnormalities in your baby. NIPT can usually only detect chromosome number abnormalities (Down's syndrome, 18-trisomy, 13-trisomy), a subset of congenital abnormalities. Some facilities offer NIPT to detect other chromosomal abnormalities, but most. Still, most chromosome number abnormalities other than the three trisomies have miscarried by the time the blood is drawn, and it has been reported that NIPT cannot find all the micro-chromosomal abnormalities that are truly pathological.
It has been said internationally that the original purpose of NIPT was to screen for three trisomies (mainly Down's syndrome) and that it is not a definitive test in prenatal diagnosis.
CRIFM has been offering "NIPT" using new technology at a low price (79,200 yen including tax).
Chromosomal abnormalities are not the only abnormalities that occur in babies. There are also abnormalities in the morphology of the brain, face, fingers, and toes, which can only be detected by an ultrasound examination of the actual baby.
For this reason, we use the "CRIFM New Prenatal Diagnosis Model," in which every patient first undergoes a "fetal dock" centered on an ultrasound examination to examine the baby and then decide whether NIPT is necessary or not.
About NIPT
NIPT, which means "non-invasive prenatal genetic testing," is a test to check for abnormalities in the chromosome number of the baby in your womb.
This test was developed to test the fetal cell-free DNA from the pregnant woman's blood to check for chromosomal abnormalities. Although there is a high positive predictive value for 21 trisomies, the positive predictive value for 18 trisomies and 13 trisomies is lower. In other words, there can be false positives (NIPT positive, but the baby does not have trisomy and is healthy). Therefore, if you test positive for NIPT, you must have a definitive test (CVS or amniocentesis).
It is also possible to test positive for micro-chromosomal abnormalities at a facility that tests for micro-chromosomal abnormalities. We receive many such consultations at our outpatient clinic specializing in NIPT positive results. However, micro-chromosomal abnormalities cannot be confirmed by the G-band test at general facilities. Still, please ensure that micro-chromosomal abnormalities can be checked appropriately by the confirmation test such as CVS or amniocentesis at CRIFM.
Position of NIPT in the medical field.
NIPT is considered a "screening test" and is therefore not a replacement for definitive tests such as amniocentesis or CVS.
Although NIPT is considered accurate, it rarely results in a false negative (a baby who tests negative for NIPT but is born with Down syndrome).
It is said that many pregnant women in the U.S. and other countries undergo NIPT. Still, the situation is entirely different from Japan, where NIPT is covered by medical insurance, and the cost for pregnant women is extremely low there.
What NIPT can tell you
NIPT can detect the presence of chromosomal number abnormalities such as trisomy 21, trisomy 18, and trisomy 13 and is available from 10 weeks in early pregnancy until late pregnancy (from 11 weeks in NIPT). The test has a higher detection rate in early pregnancy than in mid-pregnancy.
Many factors can cause congenital morphological abnormalities in the fetus, but NIPT can detect three chromosomes: trisomy 21, trisomy 18, and trisomy 13. Babies with other chromosomal trisomies will most likely be miscarried when the NIPT test is done, so it is of little use.
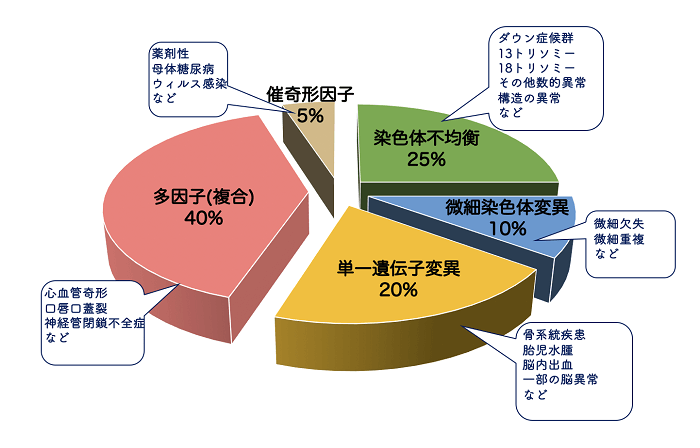
Also, since micro-chromosomal abnormalities can occur anywhere on all chromosomes, there are hundreds of possible micro-chromosomal abnormalities. Some NIPTs are supposed to detect all micro-chromosomal abnormalities, but false positives are more common than trisomies and may only add to the worry.
What is "aneuploidy (abnormal number of chromosomes)?"
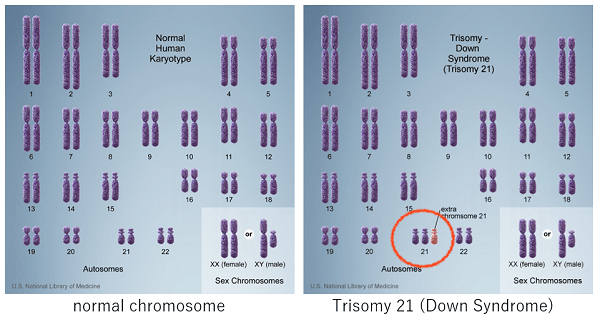
Humans have 46 chromosomes: 22 pairs of 44 autosomes (numbered 1, 2, etc.) and two sex chromosomes (X and Y).
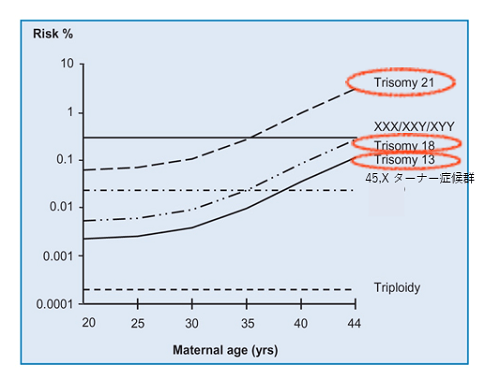
The most common type of chromosome number abnormality (aneuploidy) is called trisomy, in which there are three chromosomes instead of two. Of these, the trisomies that can be born are 21 trisomy (Down syndrome), 18 trisomy (Edwards syndrome), and 13 trisomy (Patau syndrome), and their frequency increases as the mother get older.
There are trisomies other than these, but most result in a miscarriage early in pregnancy (so there is not much point in testing NIPT to find out all the chromosome numbers). Abnormalities in the number of sex chromosomes and triploidy, which are three chromosomes in all chromosomes, have a certain frequency regardless of maternal age. It has also been reported that as mothers get older, their own sex chromosomes may become Turner mosaicism.
There are various types of chromosomal abnormalities, including mutations in the number and structure of chromosomes. This section will discuss the most common chromosome number mutations: 21 trisomy (Down syndrome), 18 trisomy, and 13 trisomy.
Even if the chromosome mutation site is the same, the symptoms, severity, and course of the disease after birth vary widely, and there are considerable individual differences. Treatment of complications associated with these chromosome mutations is available at various centers, and support groups are also functional.
What is Trisomy 21?
| Chromosomal abnormality | Trisomy 21 |
|---|---|
| Incidence | 1/691births (K.B.Sheets,2011) |
| Complications | Congenital heart disease(50%) Congenital digestive tract disorders (10%) Thyroid disease, otolaryngological disease, ophthalmological disease, mild to moderate intellectual disability |
| Prognosis | Average life expectancy The 40s to 50s |
| Support | Japan Down Syndrome Society Osaka Down Syndrome Parents' Association (in each prefecture) |
Trisomy 21, also known as Down's syndrome, occurs in about 1 out of every 2,000 mothers when the mother is 20 years old at the time of delivery, but in about 1 out of every 100 mothers when the mother is 40 years old, and the incidence increases as the maternal age increases.
Trisomy 21 is caused by an extra chromosome 21. Physical characteristics such as a slightly larger head and slightly shorter arms and legs, short stature, distinctive facial features, and developmental delay often appear.
Heart abnormalities are also seen in about half of the cases, and other complications may also be seen.
Support for Children with Trisomy 21 and their Families
Trisomy 21 (Down's Syndrome), the degree of disability varies greatly from individual to individual. Still, there is a decrease in muscle tone after birth, resulting in poor feeding and slow motor development. Because of their softness and lack of muscle tone, baby exercises that stimulate the body and help build muscle strength are recommended.
In addition, more and more children begin to receive medical care and education in the community around preschool age. It is a great way to learn how to interact with your child.
Most parents who learn of their child's illness after birth also experience mental depression and anxiety.
To help them, some university hospitals and pediatric hospitals hold parent-child classes for parents and their children to learn about the disease and interact with other families with Down syndrome. It has been found that these efforts help stabilize the parents' mental health and positively affect the parent-child relationship and the child's development.
What is Trisomy 18?
| Chromosomal abnormality | Trisomy 18 |
|---|---|
| Incidence | 1/3500~8500 births Male: Female=1:3 |
| Complications | Growth disorder, severe developmental delay, physical feature, congenital heart disease, pulmonary hypertension, respiratory complications, urinary complications, skeletal complications, deafness, malignancy |
| Prognosis | 1-year survival rate:5-10% Long-term survivors: 15 patients from 10 to 21 years old (Kosho, 2010) The main cause of death: congenital heart disease, pulmonary hypertension |
| Support | 18 Trisomy Association SOFT(USA) |
After trisomy 21, trisomy 18 has the second-highest incidence, with about 1 in 3,500 to 8,500.
About 60% of fetuses with trisomy 18 die in utero. The life expectancy after birth is also extremely short, about 1.6 months for boys and about 9.6 months for girls.
Even if you can give birth to a baby with trisomy 18, the baby will often be born with low birth weight and prone to growth and movement disorders.
Physical characteristics such as the small jaw, protruding occiput, bilateral eye segregation, hand polymerization, and limb contractures are also common.
What is Trisomy 13?
| Chromosomal abnormality | Trisomy 13 |
|---|---|
| Incidence | 1/5000 births |
| Complications | Cleft lip and palate, polydactyly, congenital heart disease, and holoprosencephaly |
| Prognosis | Average life span: 3 to 4 months Long-term survival cases: 19 years old (Japan), the 30s (Europe and US) |
| Support | Parents' Association for Children with Trisomy 13 |
Trisomy 13, also known as Patau syndrome, is a chromosomal abnormality caused by an extra duplication of chromosome 13. Its incidence is estimated to be about 1 in 5,000 to 12,000 people.
Trisomy 13 is characterized by abnormalities in various body parts such as stunted growth, severe brain diseases, facial disorders, heart diseases, and polydactyly on the side of the little finger. Still, the degree of the disease varies greatly from person to person.
The life expectancy is poor, and many die in utero during early to mid-pregnancy. It is rare for a baby with trisomy 13 to make it to the point of birth, but it is tough for them to live long after birth.
Postnatal Medical Care for Trisomy 18 and Trisomy 13
Trisomy 18 and Trisomy 13 were once thought to be diseases with no prognosis, and it was generally believed that invasive treatment after birth would be painful for the family and the child and that treatment should not be actively pursued. However, it is known that 5-10% of children with 18 trisomy reach the age of 1 year without any special treatment.
After birth, there is a severe delay in intellectual and motor development, but some children can smile and respond with understanding as development progresses.
In addition, there is information that surviving children with trisomy 18,13 develop slowly but surely, and the perception that it is not a fatal disease is changing. Even in Japan, some facilities are considering aggressive treatment, and some cases are showing positive results.
Many medical professionals are troubled by this kind of treatment policy, and as one solution, "Decision Making from an Ethical Perspective in Neonatal Care" by Nishida (1987).
However, to reflect on the paternalism of the classification from the perspective of the medical staff, in 2005, the "Guidelines for Discussions between Families of Seriously Ill Newborns and Medical Staff" was proposed. Based on these guidelines, medical staff and parents need to discuss individual responses in consideration of the child's best interests.
What are other chromosomal trisomies?
Most babies with chromosome trisomies other than chromosomes 21, 18, and 13 will be miscarried when the NIPT test is done, so there is little point.
If NIPT results show other chromosomal trisomies, they are often mosaic (normal chromosomes mixed with trisomy cells). The mosaicism is often due to trisomy cells in the placenta only, and the baby is perfectly healthy.
If you have received a result of trisomy other than chromosomes 21, 18, and 13 from NIPT at an unlicensed facility, you may want to have a fetal dock at CRIFM.
What are microchromosome abnormalities (microdeletions and microduplications)?
Some facilities offer a test that identifies five micro-chromosome abnormalities. Still, in fact, most of the babies who were found to have micro-chromosome abnormalities after microarray testing at CRIFM had micro-chromosome abnormalities other than these five. Also, many of the so-called pathogenic microdeletion/microduplication syndromes are 1-3 Mb (megabase pairs) in size. However, those found in facilities that claim to be able to detect all micro-chromosomal abnormalities by NIPT are larger deletions/duplications of 7 Mb or more. In other words, it is quite possible that important pathological sites may be overlooked.
In addition, microdeletions are occasionally benign and inherited from either parent, or they may be from placental mosaicism. It is necessary to extract the DNA from the amniotic fluid without "culture" (uncultured) and perform SNP microarray on the trio-based (parents and baby)in cases of NIPT positive microdeletion/microduplication. In other countries’ laboratories, it is common practice to deal with amniotic fluid and extract DNA in uncultured conditions. However, in general, this is still not done in other Japanese laboratories.
At CRIFM, DNA is extracted within a few hours after tissue collection by CVS or amniocentesis. Further, we use the latest technology called D-karyo to detect all micro-chromosomal abnormalities of 1Mb or more.
Advantages and disadvantages of NIPT
NIPT has both advantages and disadvantages, and it is important for couples considering NIPT to know the advantages and disadvantages of NIPT before they decide to have it. For example, having NIPT because your baby has a thick neck swelling (NT) is the wrong choice; babies with thick NTs have many abnormalities that cannot be detected by NIPT.
Advantages of NIPT
The most important advantage of NIPT is that it can test for some chromosomal abnormalities in the baby before birth using only maternal blood (non-invasive).
NIPT can test for abnormalities in chromosomes 21, 18, and 13. These three chromosomal abnormalities are said to occur more frequently in older pregnant women and can be detected between 10-15 weeks of pregnancy. (NIPT at CRIFM can be done from 11 weeks).
Disadvantages of NIPT
There are many non-Obstetrics facilities offering NIPT these days in Japan. Since they are not OB/GYNs, they are drawing blood without checking the baby. If you are going to have NIPT at a facility other than an OB/GYN, it is better to have the baby checked properly by an OB/GYN.
I once had a patient whose baby had already died in the uterus when she had NIPT at cosmetic surgery clinic.
If you get a positive result from NIPT, you will have a lot of anxiety about it. Since the test is based on a very small amount of the fetal DNA in the maternal blood, it is impossible to accurately diagnose whether the baby has a chromosomal abnormality or is growing up without any problems without actually examining the baby and performing a chromosome test.
Because it is not a definitive test, the disadvantage of NIPT is that mothers and fathers are left in limbo when the test result is positive.
Also, since NIPT is a free medical treatment, some medical institutions charge a lot of money for it. In Japan, the actual cost to the pregnant woman is around 90,000 yen to 210,000 yen for the Down Syndrome, 18 Trisomy, and 13 Trisomy tests alone, and even higher if micro-chromosomal abnormalities are included. This high cost is one of the disadvantages of NIPT, even though it is not a definitive test. NIPT by CRIFM is a highly accurate method using new technology, but the cost is 72,000 yen plus tax, which is low in Japan.
How to detect chromosome number abnormalities in a baby
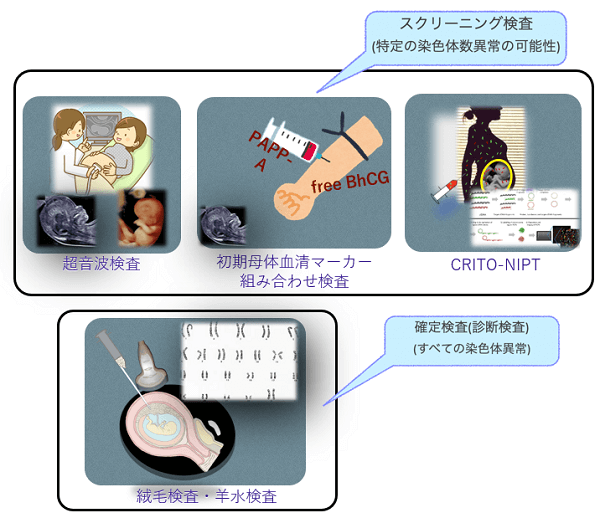
There are two ways to detect chromosomal abnormalities in babies: screening tests and definitive tests (diagnostic tests).
Screening tests are used to determine the likelihood of chromosomal abnormalities and include ultrasound (genetic ultrasound screening), early maternal serum marker combination test, and NIPT.
The screening method looks for a specific number of chromosomal abnormalities. The definitive test is to check the fetal cells in the chorionic villi (placenta) and amniotic fluid to see if there is indeed a chromosomal abnormality.
In addition to Down's syndrome, 18 trisomy, and 13 trisomy, other structural abnormalities such as chromosome number abnormalities and partial chromosome abnormalities are also detected in the definitive test. All chorionic villus examinations and amniotic fluid examinations at CRIFM use digital chromosomes (D-karyo) to check for micro-chromosomal abnormalities.
What is DNA?
DNA is a nucleic acid composed of deoxyribose (a pentose sugar), phosphoric acid, and bases. There are four types of bases: adenine, guanine, cytosine, and thymine, abbreviated as A, G, C, and T, respectively. A nucleoside with a base attached to the 1' position of the deoxyribose is called a deoxynucleoside, and a nucleoside with phosphate is attached to the 5' position of the deoxyribose is called a deoxynucleotide.
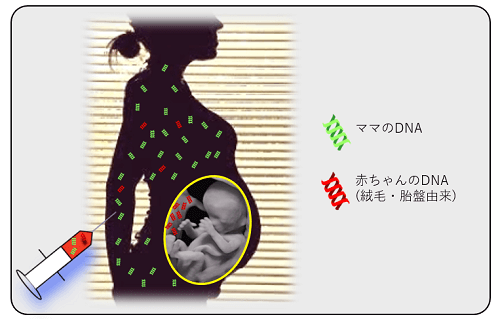
The presence of the fetal DNA in the maternal plasma was first reported by Dennis Lo et al. in 1997. As shown in the figure above, maternal blood contains fetal DNA from the beginning of pregnancy.
How the NIPT test works
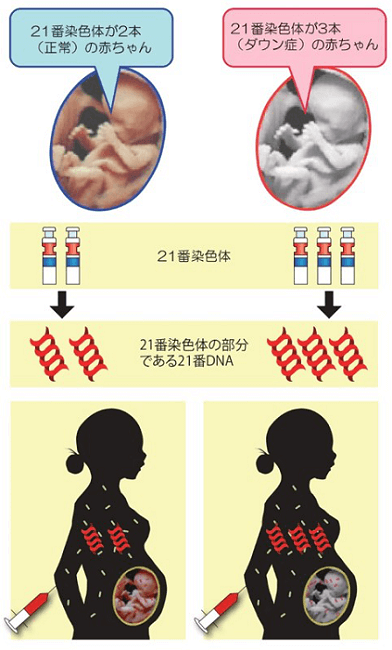
Babies with Down syndrome have three "chromosome 21," which normally has only two chromosomes. This means that when a baby with Down syndrome is in the maternal uterus, the amount of DNA in chromosome 21 is 1.5 times greater than in a normal baby.
NIPT analyzes the DNA fragments of the fetal cells in the maternal blood to check for abnormalities in the amount of DNA on chromosome 21. The amount of fetal chromosome 21 DNA in the maternal blood is very small, and even if there is an abnormality, it is a very small difference, but NIPT uses a new technology called next-generation sequencing or other technologies to detect this very small difference in the amount of DNA.
In addition, 21 trisomy (Down's syndrome), which has three chromosomes 21, tends to be focused on in older pregnancies, but theoretically, the percentage of 12-week Down's syndrome fetuses can be divided by the age of the pregnant woman as shown in the figure below.
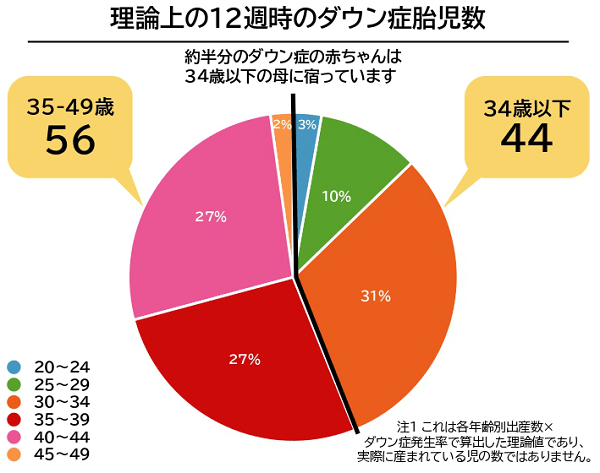
Although it is a theoretical figure, it is said that about half of all babies with Down syndrome are carried by mothers under the age of 34.
In a statement by the International Society for Prenatal Diagnosis (ISPD)
"Risk assessment based on maternal age alone is not justified.
"Early ultrasound is also inadequate in the case of NT alone.
NIPT is used for high-risk individuals.
There seems to be no disagreement with the data that NIPT is effective in high-risk individuals and that false negatives and false positives are very rare.
One of the advantages of NIPT is that the test can be done using only the pregnant woman's blood, but the diagnosis is based only on the results of the blood draw without ever seeing the baby. This can cause confusion and anxiety in pregnant women.
It is up to the patient to decide whether or not NIPT will truly relieve her anxiety and whether or not to undergo NIPT. It is the mom and dad's decision based on what the precise ultrasound will reveal.
About the NIPT test at CRIFM
NIPT is a genetic test intended to measure the fetal DNA present in maternal plasma. The patient's written consent is required for this genetic test to be performed. Here is a simple explanation of the NIPT test that we offer at CRIFM.
Based on the detailed ultrasonography of CRIFM, NIPT is being performed using the CRIFM New Prenatal Diagnostic Model, which is different from the screening that is usually done.
What is the position of NIPT?
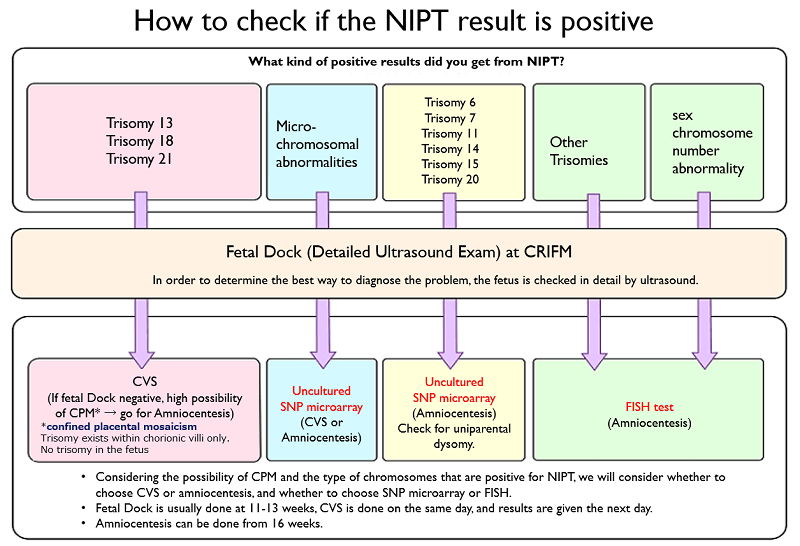
NIPT may be perceived as a first-line screening option in early pregnancy. Since many of the false positives, false negatives, and chromosomal abnormalities other than trisomy are identified in the fetal dock, CRIFM advocates the CRIFM-New Prenatal Diagnostic Model, and the first choice is a detailed ultrasound. After screening at the fetal dock, the fetus is sorted, as shown in the figure below, and the patient decides through counseling which tests to proceed to next.
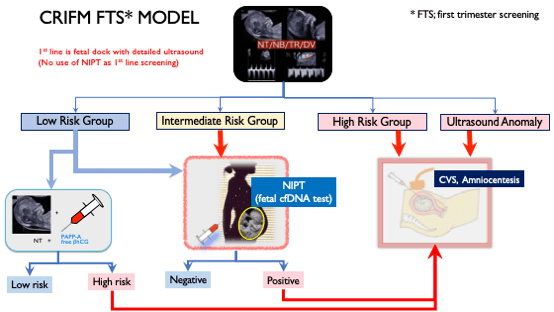
The screening method can be done in the first trimester.
At CRIFM, the early ultrasound is done between 11 and 13 weeks of pregnancy. In general, NIPT can be done from 10 weeks of pregnancy, but NIPT can be done from 11 weeks onwards because we do an early dock to identify the risk groups and determine if NIPT is indicated depending on the fetal condition. CVS can be done from 11-14 weeks and amniotic fluid examination from 16 weeks onwards.
The ultrasound screening and early serum marker combination tests give results on the same day, while NIPT takes about 7-10 days after the blood is drawn. For CVS and amniocentesis, the results for Down syndrome, 18 trisomy, and 13 trisomy are available the next day (the day of the next clinic).
NIPT is considered to have a high detection rate, but by no means can it detect all 21, 18, and 13 trisomy cases. (Although NIPT has a very high negative predictive value, it does not have a 100% positive predictive value.
A positive result in NIPT must be confirmed by amniocentesis or CVS. (Basically, NIPT is based on cfDNA from chorionic villi (placenta), so an amniotic fluid test is recommended to confirm that the baby is indeed positive.)
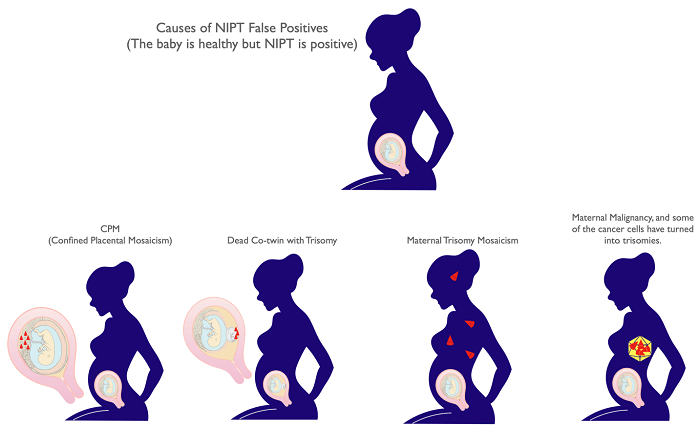
There are four possible reasons for a false-positive result, such as confined placental mosaicism or mosaicism in the mother herself. If the result is positive for NIPT, an amniotic fluid test will be done to confirm whether the baby is positive or negative, and the maternal own blood chromosome test will be done to check for trisomy in the mother herself.
If the result is positive, it does not make sense to repeat the NIPT test to reconfirm the result. It is also possible, although very rare, to have a false negative (a negative result on NIPT even though the baby has Down syndrome). However, at CRIFM, we do a detailed fetal exam before deciding whether to proceed with NIPT, so the chance of a false negative is much lower than reported.
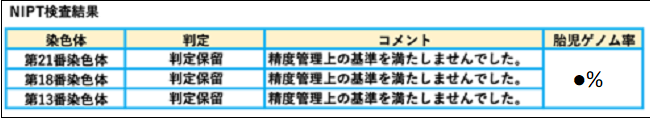
NIPT may result in a no-call (no result), in which case , it is necessary to consult again on possible subsequent actions that could be taken. Pregnant women with a high BMI may have a higher risk of no call or no result. Placental focal mosaicism and vanishing twin (one of the twins did not grow early in the pregnancy) may also be difficult to determine.
Things to keep in mind
- NIPT targets only three autosomal chromosomes (chromosomes 13, 18, and 21)
- the NIPT test does not tell you fetal gender.
- NIPT does not detect structural abnormalities such as balanced translocations, microdeletions, small but significant numerical abnormalities, fetal chromosome mosaicism, fetal genetic diseases, placental localized mosaicism, etc.
- NIPT is not designed for multiple births or vanishing twins (multiple births in which the baby has died early in the pregnancy or multiple births in which there is only a fetal sac in which the baby has not grown).
- NIPT is intended to detect specific chromosomes (chromosomes 13, 18, and 21), but it is a non-definitive test. It indicates a high probability of numerical chromosomal abnormalities and does not lead to a definitive diagnosis.
- In the case of a positive result, a definitive test such as an amniotic fluid test is always necessary to confirm the diagnosis. It has also been reported that NIPT can produce false-negative results, although this is rare. However, in the case of false negatives was found to have Trisomy 21 in the initial dock of the clinics, so it is recommended to proceed to definitive testing instead of NIPT in cases of high risk in the First Sreening.
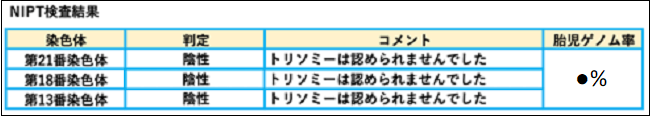
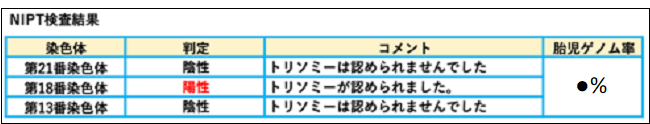
The results will be listed as negative or positive as follows.
Is there a time when NIPT is positive, but the baby is not sick?
When NIPT is positive, but the baby is not trisomic, it is called a false positive. You should be aware that NIPT can be positive in the following four cases. In the case of a positive NIPT result, we will do a definitive test and also check the maternal blood.
What should I do if I get a positive result at other clinics?
A positive NIPT result does not necessarily mean that the baby has a chromosome number abnormality, but a positive NIPT result or a no-call means that the baby must proceed to a chorionic or amniotic fluid test.
Basically, NIPT is based on cfDNA from the chorionic villi (placenta), so amniocentesis is recommended to confirm that the baby is indeed positive.
What to do if you have a positive NIPT result at another facility
A positive result on NIPT is not a definitive result.
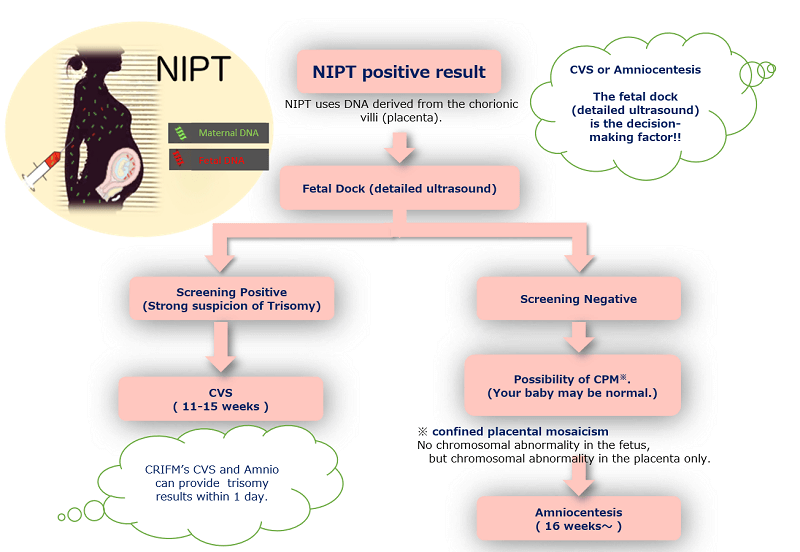
If you have a positive NIPT result, it could be a false positive, as mentioned above. The fetal dock (baby dock) can determine to some extent whether it is a false positive or a positive result.
If you have had NIPT at another facility and have a positive result, the first thing we do when you come to the "NIPT Positive Outpatient Clinic" is a fetal dock. This will determine whether to proceed to a chorionic examination or an amniocentesis.
There are also many patients who come to us because they have tested positive for chromosomal abnormalities other than trisomy 13, 18, or 21 at other facilities. Depending on the type of chromosome abnormality, the traditional G-band amniotic fluid test can miss many important diseases. At CRIFM, we perform the fetal dock according to the type of chromosomal abnormality as follows, and we use different testing methods depending on the type of chromosomal abnormality. For more information, please feel free to visit us for a genetic counseling session where we will explain in simple terms.
Can you help me with my future pregnancy and delivery?

Of course. Our clinical genetic specialists (Dr. Ritsuko K. Pooh, Dr. Hideaki Chiyo, and Dr. Yoichi Matsubara, Dr Masayuki Endo) can offer genetic counseling in person or online counseling via Zoom.
In addition, we will consult directly with the specialists at each facility for deliveries to confirm whether or not they are able to accept our patients.
Before having the NIPT test
Please read the following instructions and sign the consent form if you agree to undergo the test.
- Risk to the body
The amount of blood required for the test is 20ml. The amount of blood required for the test is 10ml, which is a small amount that is not too much for a normal person to bear and is considered to be of negligible risk to the body. - Accuracy of the test
The NIPT test is a highly accurate test that uses a new method that has already been proven to be very effective. Depending on the results of this test, further genetic testing (amniocentesis or CVS) must be performed. - About the test items
This test is only performed for numerical abnormalities of fetal chromosomes 21, 18, and 13. No other chromosomes will be tested. - Protection of personal information
Test results are kept confidential by the doctor, and we manage the protection of patients' personal information. - Genetic counseling
You will be notified individually regarding your test results. Specialized genetic counseling related to the test results will be provided at our clinic. - Academic use of analysis results
The test results may be published in academic journals and papers for academic use, but personal information will be kept separate from the results and will not be leaked. - Expenses for the test
Health insurance will not be applied to this test. You will be required to pay 72,000 yen plus tax for the CRIFM-NIPT tests.
Conclusion
A statement from the International Society for Prenatal Diagnosis says the following information is essential for pregnant women to know
- At this time, NIPT can be effective if it focuses on detecting trisomy 21, 18, and 13 in the fetus.
(Professor Nicolaides of FMF says, "NIPT should focus on detecting only 21 trisomy.") - High detection rate, but not all 21,18,13 trisomy cases can be detected.
- False-positive rate is low, but sometimes false-positive results occur, so a positive NIPT result should always be confirmed by amniocentesis or chorionic villus examination.
- There are cases where the NIPT test is not clinically meaningful, and invasive testing (chorionic or amniotic) is necessary for these patients. Pregnant women, especially those with high BMI, are at increased risk of not doing the test or not getting the results.
